- Research
- Open access
- Published:
Self-reported health related quality of life in children and adolescents with an eating disorder
BMC Psychology volume 12, Article number: 242 (2024)
Abstract
Background
Eating disorders in children and adolescents can have serious medical and psychological consequences. The objective of this retrospective quantitative study is to gain insight in self-reported Health Related Quality of Life (HRQoL) of children and adolescents with a DSM-5 diagnosis of an eating disorder.
Method
Collect and analyse data of patients aged 8–18 years, receiving treatment for an eating disorder. At the start and end of treatment patients completed the KIDSCREEN-52, a questionnaire measuring HRQoL.
Results
Data of 140 patients were analysed. Children diagnosed with Anorexia Nervosa, Bulimia Nervosa, and Other Specified Feeding or Eating Disorder all had lower HRQoL on multiple dimensions at the start of treatment, there is no statistically significant difference between these groups. In contrast, patients with Avoidant Restrictive Food Intake Disorder only had lower HRQoL for the dimension Physical Well-Being. HRQoL showed a significant improvement in many dimensions between start and end of treatment, but did not normalize compared to normative reference values of Dutch children.
Conclusion
The current study showed that self-reported HRQoL is low in children with eating disorders, both at the beginning but also at the end of treatment. This confirms the importance of continuing to invest in the various HRQoL domains.
Background
Eating disorders in children and adolescents can have serious medical and psychological consequences and rank 12th on the list of physical and mental conditions amongst woman aged 15–19 years in high-income countries when looking at the global burden of disease [1, 2]. The estimated lifetime prevalence of Anorexia Nervosa (AN) in woman is 1–4% and 1–2% for Bulimia Nervosa (BN), and the epidemiology is changing, with increasing rates of eating disorders in younger children, boys and minority groups [2, 3].
The past two decades research on health-related quality of life (HRQoL) in patients with an eating disorder has increased [4,5,6,7,8]. HRQoL is a subjective evaluation of the overall health of an individual, as well as the health of underlying subdimensions of physical, psychological and social functioning [9]. Most studies have been conducted in adults and a recent review and meta-analysis both show that eating disorders are associated with significant impaired HRQoL compared with the healthy population [10, 11]. To our knowledge only one other study evaluated the impact of eating disorders on HRQoL in children and adolescents. Jenkins et al. looked at the impact of eating disorders in a group of adolescents seeking treatment for AN, BN or eating disorder not otherwise specified (EDNOS) [6]. This study reported a poorer HRQoL measured with the SF-36 Health Survey in adolescents with an eating disorder compared with adolescent norms for the Swedish population [6]. Two studies included both children and adolescents. Weigel et al. examined the association between disorder specific factors, comorbidity and HRQoL in anorexia nervosa in adolescents and adults. HRQoL was measured using the visual analogue scale (EQ-VAS) a generic scale that does not look to different HRQoL domains [12]. Ackard et al. assessed quality of life in patients diagnosed with an eating disorder, mean age at initial assessment was 20.6 years (SD 5 8.3 years), with a range of 12–53 years. Children were not assessed separatly. Other studies in children and adolescents focused on disordered eating behaviours, but not diagnosed eating disorders [4]. A review of population-based studies showed that disordered eating attitudes and behaviours were associated with lower HRQoL in children and adolescents [9]. Herpertz-Dahlmann and colleagues found a poorer HRQoL in adolescents with self-reported disordered eating, and an association between eating disorder symptoms and psychopathology [13].
Because treating an eating disorder encompasses more than weight gain alone it is important to know the possible impact of an eating disorder on HRQoL [14]. As there are still few studies on self-reported HRQoL in children and adolescents with a diagnosed eating disorder, the primary aim of this study is to gain more insight in the different domains of self-reported HRQoL in a clinical sample of children and adolescents with a DSM-5 diagnosis of an eating disorder at the beginning of treatment. In addition, changes of HRQoL between start and end of treatment were evaluated to determine whether treatment influences HRQoL and if so which domains.
Method
Participant
Data of patients who were diagnosed conform the Diagnostic and Statistical Manual of Mental Disorders (DSM) -IV-TR/DSM-5 criteria for an eating disorder, and receiving treatment between November 2006 and April 2019 at The Mutsaersstichting were used [15, 16]. The Mutsaersstichting is a mental healthcare institute specialised in eating disorders in the Netherlands where children between 0 and 18 years receive both in- and outpatient treatment. At first presentation, every patient received an extensive consultation with a child and youth psychologist, a child and youth psychiatrist and a paediatrician. Based on this information DSM-IV-TR and DSM-5 classification were made. Patients diagnosed before 2014 were rediagnosed using the DSM-5 classification, especially using the new criteria for Avoidant Restrictive Food Intake Disorder (ARFID). Subsequently, a personalized treatment plan was presented to the family. Treatment always consisted of a combination of family-based treatment, individual treatment, group treatment and physical follow-up. Data from patients who met the DSM-5 diagnosis for AN, BN, ARFID, Binge Eating Disorder (BED), or OSFED were considered eligible for analyses. Because the study specifically focused on self-reported HRQoL, only data of children between the ages of 8 and 18 were included, since for younger children the parents completed the HRQoL questionnaire. Children and adolescents who only had HRQoL reports completed by the parents were excluded. Ethical approval was obtained from the medical ethics committee of the Maastricht University Medical Centre.
Procedure
As part of the Routine Outcome Monitoring the KIDSCREEN-52 questionnaire was sent to every patient who sought treatment for an eating disorder at the Mutsaersstichting. Baseline characteristics and clinical data were collected at the start and end of treatment. At first consultation, patient characteristics including age, sex, underlying diseases, eating attitudes and behaviours, compensatory behaviour and sociodemographic data were obtained. Heart rate and blood pressure were measured with an oscillometric blood pressure machine and evaluated according to the Clinical Practice Guidline of the American Acadamy of Pediatrics [17]. In addition, a full physical examination was performed. Body Mass Index (BMI) was calculated from measured weight and height [18]. Growth charts designed by the Dutch organization for applied scientific research (TNO) were used to determine height for age (standard deviation, SD) and weight for height (SD) [19, 20]. At the end-evaluation data was collected concerning most recent height, weight, BMI and eating attitudes and behaviours.
Measures
The KIDSCREEN-52 is a validated self-report questionnaire for measuring HRQoL in European children between 8 and 18 years old [21,22,23,24,25]. It consists of 52 questions, divided into 10 dimensions: Physical Well-being, Psychological Well-being, Moods and Emotions, Self-Perception, Autonomy, Parent Relations and Home Life, Social Support and Peers, School Environment, Social Acceptance (Bullying), and Financial Resources. The KIDSCREEN-52 uses 5-point Likert scale responses, within each different dimension the results are converted into a Rasch scale. Cronbach–alpha’s vary between 0.77 and 0.89 [25]. The results are transformed to a t-score, giving the children in the total reference population a mean t-score of 50 with a SD of 10. Specific reference populations are made by country, gender and age groups. The results of this study are compared with the validated normative reference values of Dutch children in the age between 8 and 18 years old [25]. Ulrike Ravens-Sieberer defined a mean t-score 0.5 SD below the mean t-score of the specific referential population of a country as a low HRQoL and a t-score 0.5 SD above the mean t-score of the referential population as high HRQoL [25].
Data analysis
All statistical analyses were performed using IBM SPSS Statistics version 25 [26]. The Mann-Withney U, χ2, and fisher exact test were used to determine whether there were statistical differences between all the children and adolescents included in this study and the children who completed the questionnaire at intake and end-evaluation. Paired t test was used to test for statistically significant differences in HRQoL between start- and end of treatment. To test the differences in t-score on the KIDSCREEN-52 stratified for DSM-classification, a one-way ANOVA and Welch test was done, with the Tukey’s Test as a post-hoc analysis. Statistically significance was considered when the result had a p value of < 0.05. Univariate regression analysis was done in the group diagnosed with AN to test whether there is an association between HRQoL and BMI, BMI SD, age, excessive exercise and binge eating. Since purging only occurred in four patients this could not be included in the analysis. Other DSM-5 diagnoses where not included due to small subgroup sample size.
Results
Baseline characteristics
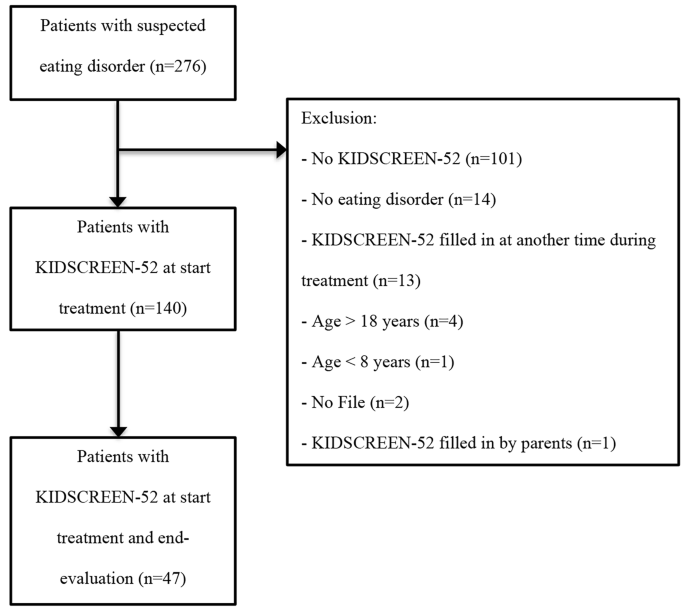
Data of 276 patients were analysed of which 140 were found eligible for this study (Fig. 1). Baseline characteristics are presented in Table 1. The total population consisted primarily of female children and adolescents (n = 119; 85%) with a mean age of 15.0 years ranging from 8 to 18 years. Almost half of the population was classified as AN (n = 68; 48.6%). The mean weight for children with AN (n = 67) was 44.1 kg (minimal weight 25 kg– maximal weight 59 kg) with a mean weight SD of -1.6 and mean BMI of 15.9 kg/m2 (minimal BMI 11.9 kg/m2– maximal BMI 19.9 kg/m2). Children with ARFID had a mean weight of 31.9 kg (minimal weight 18 kg– maximal weight 105 kg), mean weight SD– 0.6, mean BMI 15.9 kg/m2 (minimal BMI 12.1 kg/m2– maximal BMI 36.3 kg/m2). Only two patients were diagnosed with BED, this was too small a sample size to be included in results stratified for the DSM-5 criteria. No significant differences were found in the baseline characteristics between children who completed the KIDSCREEN-52 only at the beginning of treatment, and those who completed the questionnaire both at the start and end-evaluation (n = 47), except for psychiatric co-morbidities (X2 (1) = 4.97; p = 0.026). Even though the effect size for this finding, Cramer’s V = 0.188, was weak, due to the known association between psychiatric co-morbidities and eating disorder symptoms, a comparison between HRQoL at the beginning and end of treatment was only made within the group of 47 patients that completed both questionnaires [13, 27, 28].
HRQoL at the start of treatment
Table 2 shows mean t-scores scored by children and adolescents on the KIDSCREEN-52 at the start of treatment, stratified for the DSM-5 criteria. Children with the diagnosis AN, BN and OSFED all had a lower HRQoL (≤ 0.5 SD of mean score) than the reference population for the dimensions Physical Well-being, Psychological Well-being, Moods and Emotions, Self-Perception, Autonomy, Financial Resources, Peers and Social Support, School Environment and Bullying. There were no statistically significant differences in t-scores between AN, BN and OSFED. This was confirmed with a Turkey’s post hoc test. Compared with the reference population the HRQoL in patients with ARFID was only lower for the dimension Physical Well-Being. For the dimensions Physical Well-being, Psychological Well-being, Moods and Emotions, Self-Perception, Autonomy, Parent Relations and Home Life and School Environment the t-scores of children with ARFID were significantly higher than those of the children who met criteria of all other eating disorders. Social Support and Peers was significantly higher in patients with ARFID compared to AN, but not with BN and OSFED. Univariate regression analysis in the group diagnosed with AN showed a significant association between a higher t-score on the domain Physical Well-being and higher BMI, BMI SD. Other variables were not associated with a higher or lower t-score.
HRQoL change between start and end of treatment
In Table 3 mean t-scores of the KIDSCREEN-52 at the start of treatment are compared with t-scores at the end evaluation. HRQoL showed a significant improvement in mean t-scores before and after treatment for Physical Well-being (t (46) = -4.4, p < 0.001), Psychological Well-being (t (45) = − 3.0, P = 0.004), Moods and emotions (t (45) = -3.3, p = 0.002) Self Perception (t (45) = -3.7, p = 0.001) and School environment (t (44) = -2.8, p = 0.008). However, after treatment the HRQoL for these dimensions did not normalize compared to normative reference values of Dutch children. The subgroup sample sizes were too small for findings relating to change in QoL before and after treatment to be stratified by diagnosis.
Discussion
This study shows that the self-reported HRQoL in children and adolescents receiving outpatient treatment in the Netherlands for an eating disorder is significantly lower on multiple dimensions at the beginning and end of treatment compared with the reference population. Most studies that have been conducted in children and adolescents are population-based studies that focus on disordered eating behaviours, yet they also show a significantly decreased mental HRQoL [9, 13, 29,30,31,32,33,34]. The study of Jenskins, showed similar results in a group of sixty-seven adolescents seeking treatment for an eating disorder [6].
The domain physical well-being is significantly lower for all types of eating disorders. This finding replicates that of Winkler et al. in which compared to the controls, adult women with AN had significantly impaired HRQoL as measured by the Eating Disorders Quality of Life (EDQOL) scale including lower physical functioning [35]. Yet several other studies showed only a significantly lower mental component summary and normal levels in the psychical component summary scored with Short Form-36 Health Survey (SF-36) [4, 6, 14, 36]. This difference could partially be explained by the use of different questionnaires, where some questionnaires could reflect the physical pathology of eating disorders rather than real physical health. The KIDSCREEN-52 for example specifically asked for fatigue, where other questionnaires ask for the ability to walk the stairs. When diagnosed with AN extensive exercise might be associated with the disease itself. Disease severity and duration of the eating disorder might also influence results. Children and adolescents in our study received one or more previous treatments in 55% of the patients and in 34% had a disease duration of more than one year. To gain more insight a univariate regression analysis was done in the group diagnosed with AN, which showed a significant association between a higher BMI and higher t-score on the domain Physical Well-being, suggesting that the results as shown within this study might be a reflection of real physical health rather than psychopathology.
When comparing AN, BN and OSFED this study does not find statistically significant differences similar as the meta-analysis on quality of life by Winkler et al. suggesting a similarity between these eating disorders with regard to HRQoL [35]. Notable exception to this are the children and adolescents with ARFID, who only score lower on the item Physical Well-being, unlike the children and adolescents classified with all other eating disorders who have lower scores on almost all HRQoL dimensions. This suggests that HRQoL affects children with ARFID differently. Hay et al. compared adults and adolescents from the age of 15 years with ARFID in the Australian population to other eating disorders and found, unlike the current study, a normal physical HRQoL and a significantly lower mental HRQoL [37]. A Dutch study by Krom et al., in which children were treated for ARFID in a Diagnostic Centre for Feeding Problems showed that the HRQoL, reported by their parents using TNO-AZL Preschool Children Quality of Life (TAPQOL) was significantly lower on the subscales appetite, lungs, stomach, motor functioning, and positive mood and liveliness, suggesting that both physical and mental HRQoL was affected [38]. The difference in mental HRQoL between the current study and the study by Krom et al. might be explained by an overestimation by parents of the child’s psychosocial functioning due to parent’s own concerns, and besides that it might be caused by age differences. Another explanation could be that ARFID differs from longer recognised disorders such as anorexia nervosa and bulimia nervosa in that they do not have a core psychopathology of body image disturbance or weight/shape overvaluation. Given that in adolescent and young adult women at least, it is clear that overvaluation of weight/shape is very strongly associated with impairment in quality of life including but not limited to the mental health domain, it is not too surprising that children and adolescents with a diagnosis of ARFID report relatively little impairment in mental HRQoL [39, 40]. The lower physical HRQoL that is seen in the current study might be explained by nutritional deficits often seen in children with ARFID [41].
The HRQoL shows significant improvement after treatment in all dimensions except for Autonomy and Social Support and Peers. However, HRQoL does not normalize compared to the reference population, and stays significantly impaired. This finding is consistent with considerations of other studies, namely that symptom remission alone is not sufficient for improvement in quality of life [42]. Studies looking at the long-term effects of eating disorders show that the long-term HRQoL after treatment continues to improve but is still not normalized after 8- or 30-years [14, 42,43,44]. Thus follow-up, with paying attention to HRQoL, should continue longer than the initial treatment. Similar to our results, greatest improvement in HRQoL was noted in the physical functioning domain [43, 44]. With childhood and adolescence being a critical period of development, the current study underlines the importance of treatment in which the success of the treatment is not based on BMI or amount of food intake alone, but focuses on other quality of life factors, such as psychological well-being, autonomy and social support.
There are limitations to this study. Due to the small subgroup sample size findings in the change in HRQoL before and after treatment could not be stratified by diagnosis. This study enrolled participants during a 14-year period, this longer period could have confounded the results due to changes in the care and treatments. Also, the retrospective nature of this study and the use of a generic HRQoL scale needs to be taken into consideration. Using generic HRQoL scales could give an over or underestimation of the HRQoL, since it does not focus specific on eating disorders, and questions for example about physical wellbeing could be an expression of the eating disorder rather than healthy behaviour. Our patients received both in- and outpatient treatment, which implies a certain disease severity and might not be generalizable to patients in other settings. HRQoL at the start of treatment could be lower or higher depending on the setting. Even though the children who completed the KIDSCREEN-52 only at the beginning of treatment and those who completed the questionnaire both at the start and end-evaluation are comparable, a large number of patients did not fill in the KIDSCREEN-52 at end-evaluation which might influence the outcome of quality of life after treatment, especially if the patients that did recover are the ones that did not fill in the questionnaire.
However, despite the limitations this descriptive study gives insight in the self-reported HRQoL of children and adolescents in the Netherlands treated for an eating disorder. It shows a significant reduction in both mental and physical HRQoL compared to the reference population with the exception of ARFID in which only physical HRQoL is impaired. This study also shows that even after treatment, children do not achieve normal HRQoL, which poses a potential risk to their development. Long-term follow-up of these children seems important, and more research is needed focusing on the effect of using quality of life parameters as most important measurements for recovery.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- AN:
-
Anorexia Nervosa
- ARFID:
-
Avoidant Restrictive Food Intake Disorder
- BED:
-
Binge Eating Disorder
- BMI:
-
Body Mass Index
- BN:
-
Bulimia Nervosa
- DSM:
-
Diagnostic and Statistical Manual of Mental Disorders
- EDQOL:
-
Eating Disorders Quality of Life
- EDNOS:
-
Eating disorder not otherwise specified
- HRQoL:
-
Health-related quality of life
- SD:
-
Standard deviation
- SF:
-
36-Short Form-36 Health Survey
- TAPQOL:
-
TNO-AZL Preschool Children Quality of Life
References
Erskine HE, Whiteford HA, Pike KM. The global burden of eating disorders. Curr Opin Psychiatry. 2016;29(6):346–53.
Campbell K, Peebles R. Eating disorders in children and adolescents: state of the art review. Pediatrics. 2014;134(3):582–92.
Keski-Rahkonen A, Mustelin L. Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr Opin Psychiatry. 2016;29(6):340–5.
Ackard DM, Richter S, Egan A, Engel S, Cronemeyer CL. The meaning of (quality of) life in patients with eating disorders: a comparison of generic and disease-specific measures across diagnosis and outcome. Int J Eat Disord. 2014;47(3):259–67.
Engel SG, Adair CE, Las Hayas C, Abraham S. Health-related quality of life and eating disorders: a review and update. Int J Eat Disord. 2009;42(2):179–87.
Jenkins PE, Hoste RR, Doyle AC, Eddy K, Crosby RD, Hill L, et al. Health-related quality of life among adolescents with eating disorders. J Psychosom Res. 2014;76(1):1–5.
Krom H, van der Sluijs Veer L, van Zundert S, Otten MA, Benninga M, Haverman L, Kindermann A. Health related quality of life of infants and children with avoidant restrictive food intake disorder. Int J Eat Disord. 2019;52(4):410–8.
Chou B, Bohn JA, Mairs R. Acute abdominal pain caused by hematometra in an adolescent female: a case report. J Med Case Rep. 2016;10(1):369.
Wu XY, Yin WQ, Sun HW, Yang SX, Li XY, Liu HQ. The association between disordered eating and health-related quality of life among children and adolescents: a systematic review of population-based studies. PLoS ONE. 2019;14(10):e0222777.
Ágh T, Kovács G, Supina D, Pawaskar M, Herman BK, Vokó Z, Sheehan DV. A systematic review of the health-related quality of life and economic burdens of anorexia nervosa, bulimia nervosa, and binge eating disorder. Eat Weight Disord. 2016;21(3):353–64.
Winkler LA, Christiansen E, Lichtenstein MB, Hansen NB, Bilenberg N, Støving RK. Quality of life in eating disorders: a meta-analysis. Psychiatry Res. 2014;219(1):1–9.
Weigel A, Konig HH, Gumz A, Lowe B, Brettschneider C. Correlates of health related quality of life in anorexia nervosa. Int J Eat Disord. 2016;49(6):630–4.
Herpertz-Dahlmann B, Wille N, Holling H, Vloet TD, Ravens-Sieberer U, group Bs. Disordered eating behaviour and attitudes, associated psychopathology and health-related quality of life: results of the BELLA study. Eur Child Adolesc Psychiatry. 2008;17(Suppl 1):82–91.
de la Rie SM, Noordenbos G, van Furth EF. Quality of life and eating disorders. Qual Life Res. 2005;14(6):1511–22.
[APA] APA. Diagnostic and statistical manual of mental disorders: DSM-IV. (1994). Washington, DC:1994.
Association AP. Diagnostic and Statistical Manual of Mental Disorders. Diagnostic and Statistical Manual of Mental Disorders. Fifth ed2013.
Abaied JL, Wagner C, Breslend NL, Flynn M. Respiratory sinus arrhythmia as a predictor of eating disorder symptoms in college students: moderation by responses to stress and parent psychological control. Eat Behav. 2016;21:109–15.
Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284–94.
Schonbeck Y, Talma H, van Dommelen P, Bakker B, Buitendijk SE, HiraSing RA, van Buuren S. The world’s tallest nation has stopped growing taller: the height of Dutch children from 1955 to 2009. Pediatr Res. 2013;73(3):371–7.
Schonbeck Y, van Dommelen P, HiraSing RA, van Buuren S. Trend in height of Turkish and Moroccan children living in the Netherlands. PLoS ONE. 2015;10(5):e0124686.
Ravens-Sieberer U, Erhart M, Rajmil L, Herdman M, Auquier P, Bruil J, et al. Reliability, construct and criterion validity of the KIDSCREEN-10 score: a short measure for children and adolescents’ well-being and health-related quality of life. Qual Life Res. 2010;19(10):1487–500.
Ravens-Sieberer U, Gosch A, Rajmil L, Erhart M, Bruil J, Duer W, et al. KIDSCREEN-52 quality-of-life measure for children and adolescents. Expert Rev Pharmacoecon Outcomes Res. 2005;5(3):353–64.
Ravens-Sieberer U, Gosch A, Rajmil L, Erhart M, Bruil J, Power M, et al. The KIDSCREEN-52 quality of life measure for children and adolescents: psychometric results from a cross-cultural survey in 13 European countries. Value Health. 2008;11(4):645–58.
Ravens-Sieberer U, Herdman M, Devine J, Otto C, Bullinger M, Rose M, Klasen F. The European KIDSCREEN approach to measure quality of life and well-being in children: development, current application, and future advances. Qual Life Res. 2014;23(3):791–803.
Ravens-Sieberer U. The Kidscreen questionnaires: quality of life questionnaires for children and adolescents; handbook. Pabst Science Publ.; 2006.
IBM Corp. Released 2017. IBM SPSS statistics for Windows VA, NY: IBM Corp.
Padierna A, Quintana JM, Arostegui I, Gonzalez N, Horcajo MJ. The health-related quality of life in eating disorders. Qual Life Res. 2000;9(6):667–74.
Jenkins PE, Hoste RR, Meyer C, Blissett JM. Eating disorders and quality of life: a review of the literature. Clin Psychol Rev. 2011;31(1):113–21.
Ackard DM, Fulkerson JA, Neumark-Sztainer D. Psychological and behavioral risk profiles as they relate to eating disorder diagnoses and symptomatology among a school-based sample of youth. Int J Eat Disord. 2011;44(5):440–6.
Zeiler M, Waldherr K, Philipp J, Nitsch M, Dur W, Karwautz A, Wagner G. Prevalence of eating Disorder Risk and associations with Health-related quality of life: results from a large school-based Population Screening. Eur Eat Disord Rev. 2016;24(1):9–18.
Stice E, Marti CN, Shaw H, Jaconis M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. J Abnorm Psychol. 2009;118(3):587–97.
Gelin Z, Fuso S, Hendrick S, Cook-Darzens S, Simon Y. The effects of a multiple family therapy on adolescents with eating disorders: an outcome study. Fam Process. 2015;54(1):160–72.
Kenny B, Bowe SJ, Taylor CB, Moodie M, Brown V, Hoban E, Williams J. Longitudinal relationships between sub-clinical depression, sub-clinical eating disorders and health-related quality of life in early adolescence. Int J Eat Disord. 2023;56(6):1114–24.
Mitchell TB, Steele RG. Bidirectional associations between Disordered Eating and Health-Related Quality of Life in Elementary School-Age Youth. J Pediatr Psychol. 2017;42(3):315–24.
Winkler LA, Gudex C, Lichtenstein MB, Roder ME, Adair CE, Sjogren JM, Stoving RK. Explanatory factors for Disease-Specific Health-Related Quality of Life in Women with Anorexia Nervosa. J Clin Med. 2021;10(8).
Mitchison D, Hay P, Mond J, Slewa-Younan S. Self-reported history of anorexia nervosa and current quality of life: findings from a community-based study. Qual Life Res. 2013;22(2):273–81.
Hay P, Mitchison D, Collado AEL, Gonzalez-Chica DA, Stocks N, Touyz S. Burden and health-related quality of life of eating disorders, including Avoidant/Restrictive Food Intake Disorder (ARFID), in the Australian population. J Eat Disord. 2017;5:21.
Krom H, van Oers HA, van der Sluijs Veer L, van Zundert SMC, Otten MGM, Haverman L, et al. Health-Related Quality of Life and Distress of parents of children with avoidant restrictive food intake disorder. J Pediatr Gastroenterol Nutr. 2021;73(1):115–24.
Mond JM, Hay PJ, Rodgers B, Owen C. Mental health impairment associated with eating-disorder features in a community sample of women. J Ment Health. 2011;20(5):456–66.
Wagner AF, Stefano EC, Cicero DC, Latner JD, Mond JM. Eating disorder features and quality of life: does gender matter? Qual Life Res. 2016;25(10):2603–10.
Bryant-Waugh R. Avoidant/Restrictive food intake disorder. Child Adolesc Psychiatr Clin N Am. 2019;28(4):557–65.
Pohjolainen V, Koponen S, Rasanen P, Roine RP, Sintonen H, Karlsson H. Long-term health-related quality of life in eating disorders. Qual Life Res. 2016;25(9):2341–6.
Dobrescu SR, Dinkler L, Gillberg C, Rastam M, Gillberg C, Wentz E. Anorexia nervosa: 30-year outcome. Br J Psychiatry. 2020;216(2):97–104.
Padierna A, Quintana JM, Arostegui I, Gonzalez N, Horcajo MJ. Changes in health related quality of life among patients treated for eating disorders. Qual Life Res. 2002;11(6):545–52.
Acknowledgements
Not applicable.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
CRediT author statement: A Wever: Writing - Original Draft, E. van Gerner: Formal analysis and Investigation, J.C.M. Jansen: Conceptualization and Writing - Review & Editing, B Levelink: Conceptualization and Writing - Review & Editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The medical ethics committee of the Maastricht University Medical Centre was consulted for ethical approval (METC 2019 − 1027). The medical ethics committee stated that the Medical Research Involving Human Subjects Act (WMO) does not apply to this study. The need for informed consent was waived by medical ethics committee of the Maastricht University Medical Centre, because Medical Research Involving Human Subjects Act (WMO) does not apply to this study. This research was performed following the Dutch legislation that applies to retrospective research, Agreement on Medical Treatment Act (Wet op de geneeskundige behandelingsovereenkomst, WGBO, in Dutch), from the Dutch Civil Code.
Consent for publication
Not applicable.
Competing interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wever, A., van Gerner, E., Jansen, J. et al. Self-reported health related quality of life in children and adolescents with an eating disorder. BMC Psychol 12, 242 (2024). https://doi.org/10.1186/s40359-024-01684-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40359-024-01684-y