- Research
- Open access
- Published:
Influencing factors of sleep quality in pregnant: a structural equation model approach
BMC Psychology volume 12, Article number: 171 (2024)
Abstract
Background
To describe the changes in the level of sleep quality during pregnancy among pregnant women in Urumqi; also to construct a structural equation model of the factors influencing the sleep quality of pregnant women, to analyze the path relationship between the influencing factors, and to take reasonable interventions to prevent and reduce the occurrence of sleep disorders among pregnant women.
Methods
986 pregnant women who gave birth in Urumqi Maternal and Child Health Hospital and Urumqi Youai Hospital between August 2021 and May 2023 were selected. The Pittsburgh Sleep Quality Index (PSQI), Self-Rating Anxiety Scale (SAS), and Edinburgh Postpartum Depression Scale (EPDS) were used to assess the sleep, anxiety, and depression of pregnant women, Building a structural equation model based on AMOS 23.0 Tools.
Results
The results of structural equation modeling showed that: basic characteristics, obstetrical characteristics, tocolysis, lifestyle, psychological had a direct effect on the PSQI, with path coefficients of 0.243, 0.106, 0.140, 0.174, 0.658, the corresponding T-values for each path are 4.585, 2.677, 2.578, 2.297, and 9.036. The indirect effect of basic characteristics, obstetric characteristics and lifestyle on PSQI was 0.123, 0.020, 0.027.
Conclusions
The high incidence of sleep disorders in pregnant women and their close association with psychological symptoms in pregnant women should focus on screening and counseling regarding psychological disorders in pregnant women, thus improving the quality of sleep in pregnant women.
Introduction
Sleep is an indispensable life activity for human beings and an important protective mechanism, occupying almost one-third of life. Adequate and good sleep can satisfy both physical and psychological needs of human beings, as well as allow people to recover physical and mental strength and enhance work efficiency. Pregnancy is a short and unique process, due to the hormone levels during pregnancy affecting pregnant women in physical, physiological, social and psychological changes, making pregnant women more prone to insomnia, urinary frequency, frequent waking up at night and sleep deprivation, which can lead to sleep disorders and adverse pregnancy outcome [1]. In addition, socio-demographic characteristics (age, education level, economic income and BMI), mood disorders have been reported to affect the quality of sleep in pregnant women, with higher depression and anxiety scores associated with poorer sleep quality [2, 3].
Most pregnant mothers report altered sleep during pregnancy, and results from previous studies have shown a wide range in the prevalence of poor sleep quality in women during pregnancy, ranging from 29–84% [4, 5],with a mean PSQI score of 6.07 [5.30, 6.85] during pregnancy [4],Sleep quality is characterized by poorer subjective sleep quality, reduced habitual sleep efficiency, and sleep disturbances increase, and longer time to fall asleep. Chronic low-quality sleep exacerbates the risk of multiple negative perinatal pregnancy outcomes, including mood disorders [5, 6], cesarean section rate, prolonged labor and delivery, gestational diabetes mellitus [7], preeclampsia, preterm labor, and low birth weight of neonates [1, 8, 9]. It is thus clear that sleep disorders pose a serious threat to the health of both the pregnant woman and the fetus.
Given the complex interplay of these factors, a comprehensive analysis was deemed necessary to understand the current status and influences on sleep quality in pregnant women. Structural equation modeling (SEM) provides a valuable statistical method to synthesize path-reflective relationships between variables and identify the direct and indirect effects of multiple factors on sleep quality. In this study, a theoretical model was initially constructed using sleep quality as an endogenous latent variable and basic characteristics, obstetrical characteristics, tocolysis, lifestyle, and psychological status as exogenous latent variables, and the fit of the theoretical model was verified to explain and predict the factors affecting sleep quality in pregnant women to ensure that the model proposed by the investigators was supported by data under real conditions. In turn, the key factors leading to poor sleep quality were identified, healthcare professionals can implement targeted interventions and develop strategies to promote better sleep during pregnancy in order to improve the overall health of pregnant women during gestation, optimize their pregnancy experience, while promoting healthy fetal development in the womb.
Methods
Participants
The present study was a cross-sectional study in which pregnant women in pregnancy who underwent labor checkups at the obstetrics outpatient clinics of Urumqi Maternal and Child Health Hospital and Urumqi You’ai Hospital during the period of August 2021 ∼ May 2023 were selected by simple random sampling, and pregnant women who met the inclusion criteria were surveyed face-to-face with an electronic questionnaire. Firstly, the purpose, procedure and filling requirements of this survey were explained to pregnant women, and after fully understanding this study, they signed the informed consent form. At the beginning of the survey, pregnant women could choose to fill out the questionnaire independently in the hospital public number with their cell phones, and professionally trained investigators were beside them to explain the entries that were not understood by the research subjects in time; for pregnant women who were not able to answer the questionnaire independently on their cell phones, they could also choose to fill out the paper questionnaire, and fill out the questionnaire in the form of a one-question-one-answer format between the investigators and the pregnant women.
Inclusion criteria
-
(1)
Pregnant women aged ≥ 18 years;
-
(2)
Volunteered to participate in this research study and was able to complete the electronic questionnaire independently;
-
(3)
Local permanent residents (≥ 1 year of residence).
Exclusion criteria
-
(1)
Suffering from a serious mental illness;
-
(2)
Planned early termination of pregnancy;
-
(3)
Incomplete information on the questionnaire.
Data collection tools
Basic information questionnaire
The Basic Information Questionnaire collects basic information on pregnant women’s gestation period, age, height, weight, ethnicity, literacy, place of residence, occupation, husband’s information, per capita monthly household income, past medical history, maternal history, exercise, health behaviors, husband-wife relationship, in-laws’ relationship, and whether they are sociable or not.
Pittsburgh sleep quality index scale
The Pittsburgh Sleep Quality Index (PSQI) was used to evaluate the sleep of pregnant women [4]. The scale is a questionnaire containing 18 entries to measure habitual sleep quality over a recent month [10]; it consists of seven subscales assessing sleep duration, nocturnal sleep disturbances, sleep latency, sleep quality, daytime dysfunction, sleep medication use and sleep efficiency. Scores for each subscale ranged from 0 to 3, and overall scores ranged from 0 to 21. Higher scores indicate poorer sleep quality in women during pregnancy. In this study PSQI score greater than 7 indicates poor quality of sleep and less than or equal to 7 is good quality of sleep [11].The Cronbach’s α was 0.721.
Self-rating anxiety scale
The Self-Rating Anxiety Scale (SAS) was used to assess anxiety symptoms in pregnant women [12]. The scale consists of 20 items, and the scores of each item are summed to obtain a crude score, which is multiplied and rounded to 1.25 to obtain a standardized total score (SAS). In this study, a SAS greater than or equal to 50 was defined as the presence of anxiety symptoms, with higher scores indicating a more pronounced anxiety condition [13]. The Cronbach’s α was 0.733.
Edinburgh postnatal depression scale
The Edinburgh Postpartum Depression Scale (EPDS) was applied to assess depression during pregnancy [14], the scale score is obtained by summing the 10 entries included, with a total score ranging from 0 to 30, and a total EPDS score of greater than or equal to 10 was used in the study as the threshold for screening for depressive symptoms [15]. The Cronbach’s α was 0.808.
Statistical analysis
Survey data were entered using the Epidata 3.1 database, and statistical analyses were performed using IBM SPSS Statistics 27.0 (IBM Corporation, Armonk, NY, USA) and AMOS 23.0 (IBM, New York, NY, USA). For measurement information, expressed as mean ± standard deviation, t-test was used for comparison between two groups and analysis of variance (ANOVA) was used between multiple groups if normal distribution and chi-square were met; rank-sum test was used when normal distribution was not met. For the count data, expressed as frequency and percentage, the \( \chi^{2} \) test was used for comparison between groups. to describe the current epidemiologic status of sleep quality among pregnant women in Urumqi and the prevalence trends on different demographic characteristics. Spearman correlation was applied to analyze the correlation between variables. The main influences on sleep quality of pregnant women and the path relationships between them were explored through structural equation modeling, and the following goodness-of-fit indices were used to evaluate the model: λ²/df < 5, CFI > 0.90,GFI > 0.90, AGFI > 0.90, IFI > 0.90, and RMSEA < 0.05.
Moral statement
Participation in the study was voluntary and anonymous, and participants were given the option to opt out at any time while undergoing the survey to ensure that personal privacy was respected and protected. Prior to the start of the survey, all subjects signed a written informed consent to participate in the program. The study involving human subjects in this protocol was reviewed and approved by the Nutrition and Health Ethics Committee of the Chinese Center for Disease Control and Prevention (No. 2021-008), in accordance with the Declaration of Helsinki.
Results
Basic characteristic
Table 1 describes the basic characteristics of the included study population, which included 986 pregnant women, of whom 217, 471, and 298 were in the early, middle, and late stages of pregnancy, respectively. The age ranged from 20 to 47 years, with a mean age of 31.28 ± 4.25 years, 620 (62.9%) were Han, and 312 (31.6%) were predominantly educated to undergraduate level. There were 39.0% of pregnant women who had their first pregnancy and 232 (23.5%) who were on birth control. The PSQI score of pregnant women was 4.84 ± 3.12, 179 (18.2%) pregnant women had sleep disorders, 111 (11.3%) and 297 (30.1%) had symptoms of anxiety and depression, 48 (43.2%) pregnant women had both anxiety and sleep disorders, 104 (18.2%) pregnant women had both depression and sleep disorders, and there was a significant difference between both and the non-sleep disordered group. disorder group were significantly different.
Table 2 shows the overall score, component scores and depression and anxiety scores of sleep quality in women in early, mid and late pregnancy. As the course of pregnancy increased, both sleep quality scores and depression and anxiety scores showed an increasing trend, with significant differences in overall sleep quality scores across trimesters of 4.22 (3.13), 4.81 (2.97), and 5.34 (3.25), and depression scores of: 6.25 (4.90), 7.56 (4.56), and 7.56 (4.92). There were significant differences in all the indicators except Anxiety, Sleep latency, Use Hypnotic drug, Daytime dysfunction.
Correlation analysis
Table 3 shows Spearman’s correlation between socio-demographic factors, depression and anxiety and sleep quality among all participating pregnant women (n = 986). Sleep quality was correlated with education level (r = 0.129,p < 0.001), parity (r = 0.080,p < 0.05), gravidity, primiparity, vaginal bleeding, tocolysis (r = 0.099,p < 0.001), husband drinking alcohol, anxiety (r = 0.232,p < 0.001), depressed (r = 0.287,p < 0.001) were correlated. The higher the level of education, the greater the correlation between the emergence of sleep quality problems in pregnant women. Similarly, the more pronounced the expression of depression and anxiety, the increase in sleep disorders in women during pregnancy is associated. The strength of the correlation between these variables was between weak and moderate, and there was no correlation between the quality of sleep of pregnant women and their occupation and monthly income.
Structural equation model
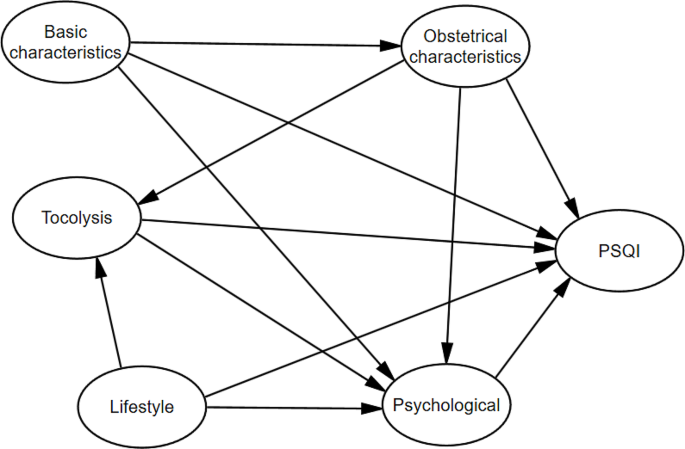
In order to reasonably and comprehensively study the changes in the level of sleep quality during pregnancy among pregnant women in Urumqi; and to explore the influencing factors of sleep quality among women during pregnancy, an initial structural equation model was established based on the results of previous studies in the relevant literature. Inclusion of study variables in exploratory factorial molecules. KMO test and Bartlet’s Sphericity test, the KMO value was 0.649 and the Bartlet ‘s sphericity test had a difference (P < 0.001) and the results showed that the data satisfied the factor analysis. The principal component analysis method was used to extract factors, in order to make the difference between the attributes of the factors is obvious, using the maximum variance rotation method to rotate the factors, the cumulative explanation of 61.62% of the variance, to get the rotated factor loadings as in Table 4, factor 1 is named obstetric characteristics (Primiparity, Parity, Gravidity), factor 2 is named basic characteristics (Monthly income, Occupation, Educatin level), factor 3 is named as tocolysis (Vaginal Bleeding, Tocolytic), factor 4 is named as psychological (Anxious, Depressed), factor 5 is named as Lifestyle (Smoke, Alcohol, Husband drinking alcohol). The initial structural equation modeling of the five variables of basic characteristics, obstetric characteristics, tocolysis, lifestyle, and psychological with sleep quality was established. As shown in Fig. 1.
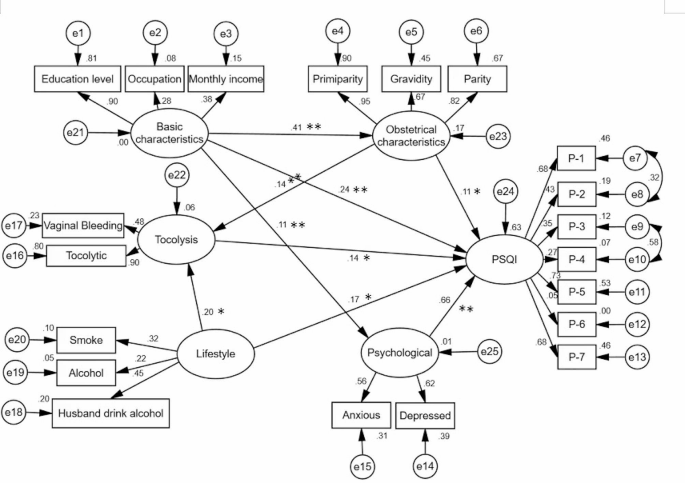
The initial model is tested and corrected, and the maximum likelihood method is chosen for parameter estimation. Comprehensive consideration of the correction index, deletion of meaningless paths and other measures after repeated modifications, the SEM model with a better fit is shown in Fig. 2. The results of the main fitting indexes show that: Chi/df = 3.038,GFI = 0.951,AGFI = 0.935,IFI = 0.926,TLI = 0.910,RMSEA = 0.046.The specific results are shown in Table 5.
The summary table of path coefficients shows that there is a direct effect of obstetric characteristics → PSQI with a path coefficient of 0.106 and a t-value of 2.677 (P < 0.001), a positive and direct effect of obstetric characteristics → tocolysis with a path coefficient of 0.142 and a t-value of 3.876 (P < 0.001), and a direct and positive effect of tocolysis → PSQI with a path coefficient of 0.140 and a t-value of 2.578 (P < 0.05). The standardized path coefficient of basic characteristics on PSQI through tocolysis was 0.020 (0.14*0.14), the indirect effect was 0.020, the direct effect was 0.106, and the total effect was 0.126. The direct and indirect effects accounted for 84.1% and 15.9% of the total effect, respectively. Thus, 15.9% of the effect of obstetrical characteristics on PSQI was through tocolysis. The direct effect of basic characteristics → PSQI was 0.243 with a t-value of 4.548 (P < 0.001) and the indirect effect was 0.123; psychological → PSQI had a direct effect with a path coefficient of 0.658 and a t-value of 9.036. lifestyle → PSQI had a path coefficient of 0.174 and a t-value of 2.297 (P < 0.05). The indirect effect of lifestyle on pregnant women’s sleep quality through birth control was 0.027,accounting for 13.43% of the total effect. See Table 6.
Discussion
Sleep disorders are common throughout pregnancy. Previous national and international studies have shown that pregnant women have varying degrees of sleep quality problems during all trimesters [16]. In this study, the mean PSQI score of all subjects was 4.84 ± 3.12, and 18.2% of pregnant women had sleep disorders. It was lower than the findings of Li [17]. who had a sleep disorder rate of 54.3%, and this difference may come from the difference in the threshold value of PSQI (PSQI > 5). Where the scores were 4.22 ± 3.13, 4.81 ± 2.97, and 5.34 ± 3.25 in early, middle, and late pregnancy, respectively, we found that PSQI scores increased with the progression of pregnancy, and that pregnant women’s sleep quality was most susceptible to disturbances in late pregnancy. Similar to the findings of Kızılırmak’s study [18]. This increasing trend may be related to poor sleep quality due to hormone levels, fetal movement, physical discomfort, and frequent nighttime bathroom visits during pregnancy [19, 20].
In this study, we found that the quality of sleep in pregnant women was also associated with age, education, whether they were primiparous, pregnancy history, and birth control. The prevalence of sleep disorders in pregnant women of higher gestational age (age ≥ 35) was 24.1%, which was higher than that of lower age, which was 17.1%. That is, the higher the maternal age, the higher the prevalence of sleep disorders during pregnancy [16, 21]. It may also be related to the fact that older women are themselves more susceptible to workplace pressures, caring for their families and children, and the concern about the higher risk of adverse pregnancy outcomes associated with advanced age, which makes their psychological burden heavier and affects their sleep [22]. We found that there is also a close relationship between the level of education of pregnant women and sleep status, undergraduate and postgraduate there is a sleep retardation rate of 49.9%, high educational level but affect the quality of sleep, to consider that it may be related to the probability of this group of people to engage in mental labor is relatively large, the pressure of the work is high, so they are more susceptible to the impactt. There is a discrepancy with the findings of Cai[5], who concluded that the higher the level of education, the more knowledge and access pregnant women acquire to regulate their sleep, leading to better sleep improvement.
The present study further explored the direct and indirect effects of sleep quality in pregnant women based on structural equation modeling with the aim of providing better interventions for better improvement of sleep quality during pregnancy. The results of the study showed that basic characteristics, obstetric characteristics,tocolysis, lifestyle, psychological had a direct effect on PSQI. tocolysis had a mediating effect between obstetric characteristics and PSQI, indicating that obstetric characteristics not only directly affect PSQI, but also indirectly affect sleep quality through tocolysis. The mediating effect was 15.9%. Parity and pregnancy history were risk factors for sleep quality. Compared to primiparous women, transient women reported poorer sleep quality, which may be related to the physical and psychological stress that exists during pregnancy itself, the fact that women also have to take care of their first child and the expectation of the gender of the second child in some families, which makes the pregnant women anxious, thus leading to poorer quality of sleep [23,24,25]. Van [26]compared the effect of comparing the presence or absence of a history of miscarriage on the quality of sleep in the later part of pregnancy in pregnant women who were pregnant during the late stage of pregnancy. showed that sleep duration (7.1 ± 1.1 h) and sleep efficiency (83.7 ± 7.9%) were similar in both groups, however, the PSQI score of the miscarriage group (7.8 ± 2.6) was significantly lower than that of the control group (6.7 ± 3.1), suggesting that having a history of miscarriage is an influencing factor in the low quality of sleep in women with a late pregnancy. At the same time, when pregnant women with vaginal bleeding and their own low back and abdominal pain receive tocolysis treatment, anxiety, anxiety and other adverse psychological emotions due to the fear of their own and fetal health, leading to poor treatment compliance and affecting the effect of sleep quality. Therefore, it is necessary to pay attention to the pregnancy history of pregnant women, and adopt the treatment of Tocolytic for pregnant women with threatened abortion, along with certain psychological guidance, to prevent the occurrence of adverse pregnancy outcomes [27].
Lifestyle has a direct effect on sleep quality (0.174), can also indirectly affect the quality of pregnant women’s sleep from tocolysis(0.027), the total effect is( 0.201). Alcohol not only harms the drinker, in the case of alcohol consumption, alcohol fluctuates moods domestic violence will rise, resulting in harm to family members and the atmosphere, foreign scholars have shown that if the husband is drinking, the woman is more likely to be subjected to domestic violence, more susceptible to physical and psychological stress, which further affects sleep [28,29,30].
In addition, pregnancy sleep quality during pregnancy is strongly associated with pregncancy’s psychological, and we found that psychological had a direct and significant effect on the quality of sleep of pregnant women with a path coefficient of 0.658. Based on previous studies, it was found that pregnant women experience high mood swings throughout pregnancy, which are accompanied by varying degrees of anxiety and stress as well as depression, and the higher the level of depression in pregnant women, the worse the quality of sleep [31, 32]. Polo-Kantola [33] confirmed a correlation between sleep quality and depression and anxiety during pregnancy. LI found a direct effect of anxiety on depression, suggesting that pregnant women with symptoms of anxiety during pregnancy have a higher risk of developing depressive symptoms [34], and therefore anxiety is one of the strongest factors that have been strongly associated with prenatal depression one of the strongest associations with prenatal depression [35]. Another study shows that depression and anxiety scores in pregnant women are important hubs for regulating the relationship between objective and subjective sleep [36]. Many pregnant women after pregnancy will have concerns about their competence as a mother, worry about their inability to complete the role transition, worry about their delivery and infant feeding methods and the hopes of relatives for pregnant women can produce pregnancy-related anxiety and anxiety, which [37], if appropriate interventions are not taken, will potentially lead to adverse consequences of postpartum depression.
Conclusions
The results of this study indicate that sleep quality problems are prevalent among pregnant women in Urumqi and increase with the trimester of pregnancy. Considering the path relationships between the variables, basic characteristics, obstetric characteristics, tocolysis, lifestyle、psychological were found to be influential factors for sleep quality, especially the impact of psychology on the sleep quality of pregnant women is particularly significant. Therefore, healthcare organizations should pay attention to screening pregnant women for sleep disorders and psychological disorders, and develop reasonable and effective interventions to reduce the incidence of adverse pregnancy outcomes caused by sleep disorders.
Limitations
Our research also has certain limitations. Firstly, due to cross-sectional design, it is limited to comprehensively explore the influencing factors of sleep quality in pregnant women; Secondly, our research did not consider social support factors, which may have a certain impact on our results; Finally, the scale for evaluating sleep quality, depression and anxiety in this study was objectively filled out by pregnant women, and there may be some recall bias.
Data availability
The authors will supply the relevant data in response to reasonable requests.
References
Lu Q, Zhang X, Wang Y, et al. Sleep disturbances during pregnancy and adverse maternal and fetal outcomes: a systematic review and meta-analysis. Sleep Med Rev. 2021;58:101436.
Wang Y, Liu H, Zhang C, et al. Antepartum sleep quality, mental status, and postpartum depressive symptoms: a mediation analysis. BMC Psychiatry. 2022;22(1):521.
Tomfohr LM, Buliga E, Letourneau NL, et al. Trajectories of Sleep Quality and associations with Mood during the Perinatal Period. Sleep. 2015;38(8):1237–45.
Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Cai S, Tan S, Gluckman PD et al. Sleep Quality and Nocturnal Sleep Duration in Pregnancy and Risk of Gestational Diabetes Mellitus. Sleep. 2017; 40(2)
Pauley AM, Moore GA, Mama SK, et al. Associations between prenatal sleep and psychological health: a systematic review. J Clin Sleep Medicine: JCSM: Official Publication Am Acad Sleep Med. 2020;16(4):619–30.
Reutrakul S, Anothaisintawee T, Herring SJ, et al. Short sleep duration and hyperglycemia in pregnancy: aggregate and individual patient data meta-analysis. Sleep Med Rev. 2018;40:31–42.
Warland J, Dorrian J, Morrison JL, et al. Maternal sleep during pregnancy and poor fetal outcomes: a scoping review of the literature with meta-analysis. Sleep Med Rev. 2018;41:197–219.
Xu T, Feng Y, Peng H, et al. Obstructive sleep apnea and the risk of perinatal outcomes: a meta-analysis of cohort studies. Sci Rep. 2014;4:6982.
Okun ML, Mancuso RA, Hobel CJ, et al. Poor sleep quality increases symptoms of depression and anxiety in postpartum women. J Behav Med. 2018;41(5):703–10.
Mao XF, Shao L, Zhao X, et al. Sleep quality and influencing factors of perimenopausal women in Ningbo region. J Zhejiang Univ Med Sci. 2011;40(1):85–9.
Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–9.
Roberson EK, Hurwitz EL, Li D, et al. Depression, anxiety, and Pharmacotherapy around the time of pregnancy in Hawaii. Int J Behav Med. 2016;23(4):515–26.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry: J Mental Sci. 1987;150:782–6.
Lee DT, Yip SK, Chiu HF, et al. Detecting postnatal depression in Chinese women. Validation of the Chinese version of the Edinburgh postnatal depression scale. Br J Psychiatry: J Mental Sci. 1998;172:433–7.
Sedov ID, Cameron EE, Madigan S, et al. Sleep quality during pregnancy: a meta-analysis. Sleep Med Rev. 2018;38:168–76.
Li P, Wang H, Chen G, et al. Association between Nausea and vomiting during pregnancy and Sleep Quality: Mediating Effect of depressive symptoms. Int J Gen Med. 2021;14:41–9.
Kızılırmak A, Timur S, Kartal B. Insomnia in pregnancy and factors related to insomnia. TheScientificWorldJournal. 2012; 2012:197093.
Hutchison BL, Stone PR, McCowan LM, et al. A postal survey of maternal sleep in late pregnancy. BMC Pregnancy Childbirth. 2012;12:144.
Tan L, Zou J, Zhang Y, et al. A longitudinal study of physical activity to improve Sleep Quality during pregnancy. Nat Sci Sleep. 2020;12:431–42.
Jemere T, Getahun B, Tadele F, et al. Poor sleep quality and its associated factors among pregnant women in Northern Ethiopia, 2020: a cross sectional study. PLoS ONE. 2021;16(5):e0250985.
Signal TL, Paine SJ, Sweeney B, et al. Prevalence of abnormal sleep duration and excessive daytime sleepiness in pregnancy and the role of socio-demographic factors: comparing pregnant women with women in the general population. Sleep Med. 2014;15(12):1477–83.
Cai Y, Shen Z, Zhou B, et al. Psychological Status during the second pregnancy and its influencing factors. Patient Prefer Adherence. 2022;16:2355–63.
Christian LM, Carroll JE, Porter K, et al. Sleep quality across pregnancy and postpartum: effects of parity and race. Sleep Health. 2019;5(4):327–34.
Du M, Liu J, Han N, et al. Maternal sleep quality during early pregnancy, risk factors and its impact on pregnancy outcomes: a prospective cohort study. Sleep Med. 2021;79:11–8.
Van P, Gay CL, Lee KA. Prior pregnancy loss and sleep experience during subsequent pregnancy. Sleep Health. 2023;9(1):33–9.
Ota H, Hasegawa J, Sekizawa A. Effect of sleep disorders on threatened premature delivery. J Perinat Med. 2017;45(1):57–61.
Bhatta N, Assanangkornchai S, Rajbhandari I. Does husband’s alcohol consumption increase the risk of domestic violence during the pregnancy and postpartum periods in Nepalese women? BMC Public Health. 2021;21(1):5.
Gebrezgi BH, Badi MB, Cherkose EA, et al. Factors associated with intimate partner physical violence among women attending antenatal care in Shire Endaselassie town, Tigray, northern Ethiopia: a cross-sectional study, July 2015. Reproductive Health. 2017;14(1):76.
Viellas EF, Gama SG, Carvalho ML, et al. Factors associated with physical aggression in pregnant women and adverse outcomes for the newborn. Jornal De Pediatria. 2013;89(1):83–90.
Yang Y, Mao J, Ye Z, et al. Determinants of sleep quality among pregnant women in China: a cross-sectional survey. J maternal-fetal Neonatal Medicine: Official J Eur Association Perinat Med Federation Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2018;31(22):2980–5.
Yu Y, Li M, Pu L, et al. Sleep was associated with depression and anxiety status during pregnancy: a prospective longitudinal study. Arch Women Ment Health. 2017;20(5):695–701.
Polo-Kantola P, Aukia L, Karlsson H, et al. Sleep quality during pregnancy: associations with depressive and anxiety symptoms. Acta Obstet Gynecol Scand. 2017;96(2):198–206.
Li Y, Zeng Y, Zhu W, et al. Path model of antenatal stress and depressive symptoms among Chinese primipara in late pregnancy. BMC Pregnancy Childbirth. 2016;16(1):180.
Lancaster CA, Gold KJ, Flynn HA, et al. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202(1):5–14.
Volkovich E, Tikotzky L, Manber RJA. Objective and subjective sleep during pregnancy: links with depressive and anxiety symptoms. 2016; 19:173–81.
Bao C, Jin D, Sun S, et al. Trajectories and depressive symptoms during the Perinatal period: a Longitudinal Population-based study in China. Front Psychiatry. 2022;13:762719.
Acknowledgements
We sincerely thank all the pregnant women and staff who participated in this study.
Funding
This work has been funded by the National Natural Science Foundation of China funded projects (72163033).
Author information
Authors and Affiliations
Contributions
MB: conceptualization, writing– original draft, writing– review & editing. YZ and YG: Collect the data. MB, SH and DW: statistical analysis, editing the manuscript. LZ: editing and review the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee of the Nutrition and Health Ethics Committee of the Chinese Center for Disease Control and Prevention (CDC) reviewed and approved the protocol, No. 2021-008.Informed consent signed by all participants prior to the survey.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bahani, M., Zhang, Y., Guo, Y. et al. Influencing factors of sleep quality in pregnant: a structural equation model approach. BMC Psychol 12, 171 (2024). https://doi.org/10.1186/s40359-024-01657-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40359-024-01657-1